We need to "measure what matters" as the saying goes. As we move to new payment models, we'll need to develop platforms that are designed to measure and learn from a wide array of data points about what works in keeping people healthy. Of course, we'll need health care architectures that can support big data across a wide variety of platforms to enable better algorithms and more learning. There's certainly big opportunity for connecting all these systems.
But it's not just the connection of data in and of itself that will lead to improvements in the triple aim of care, health and costs...Health IT architecture itself can improve the likelihood of cost savings. We need to look deeper at the IT platform as a risk-reducer that can significantly reduce health care costs. Could we one day have an actuarial field of study in the network science in health care?
What do I mean by this? How do architectures reduce risk? Well, mostly by connecting problems with solutions, but in other ways as well. Let's explore this a bit.
When I say an architecture can reduce risk, I'm largely referring to a web 2.0 approach. https://radar.oreilly.com/2005/10/web-20-compact-definition.html
O'Reilly's short Web 2.0 Definition.
"Web 2.0 is the network as platform, spanning all connected devices; Web 2.0 applications are those that make the most of the intrinsic advantages of that platform: delivering software as a continually-updated service that gets better the more people use it, consuming and remixing data from multiple sources, including individual users, while providing their own data and services in a form that allows remixing by others, creating network effects through an "architecture of participation," and going beyond the page metaphor of Web 1.0 to deliver rich user experiences."
That's all great, but what's missing is how, beyond the data that can be collected, these architectures reduce risk by their very nature of sharing and connecting. This is an area that I expect will be explored deeply and continually quantiifed as we move to new payment mechanisms in health care. I believe 2.0 architecture and platforms will be required for accountable care to succeed. Here's why.
How do these platform architectures reduce risk?
They create a kind of planned serendipity where problems and solutions come together. We'll need to find a way to measure this effect.
To understand this a little better, let's tak a look at the Birthday Paradox.(This is something I learned back in my Probability and Statistics 101 and Clay Shirky also writes about this concept in Here Comes Everybody, The Power of Organizing without Organizations) The Birthday Paradox goes a long way to explaining why social media, markets, open source and more open platform architectures work. Ironically, Accountable Care Organizations will be dependent on this type of organizing without organizations. Here it is.
What are the chances that you and another person chosen at random have the same birthday?
OK, pretty easy one. It's more or less 1 in 365 (not including off chance of a leap year birthday).
Now, take 36 people and put them in a room. What are the chances that there are 2 people in the room with the same birthday?
If you're like most people, you'd take a back o' the napkin guess of about 10-30%, but once again, our statistical intuitions betray us. We tend to think of individuals rather than matching pairs. Yes, it's about a 10% chance that YOU will find someone else in the system with your birthday, but it's an 80% chance that there will be one pair with the same birthday in the group, an increase in a likelihood of 1 in 365, or 0.27%, to a likelihood of 80% by connecting (by putting them in the same group) 36 few people. That's a 300-fold increase in probability of at least one match in the group.
The likelihood of finding a pair rises with the square of the number in the group, it's a principle of markets, of social networks and collaborative systems design.
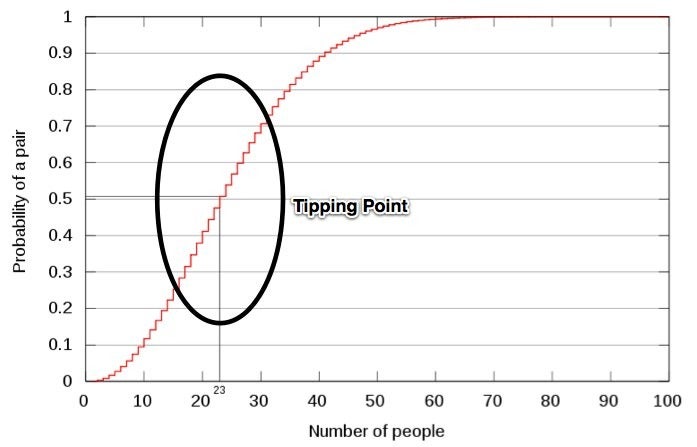
Let's say that instead of trying to match up people with the same birthdays, we're looking to match up a piece of a code where it could be reused, or perhaps match up a specialist with someone with a rare medical condition, or matching an investor with a great investment or a patient with a clinical trial. It works for any kind of matching in a population, all it takes is getting the parties on the same platform and enabling communication.
A 300-fold or a million-fold increase in probability means the Birthday Paradox has a real quantifiable value, and that's just the value of the first step of finding each other.
Note: Of course, in most real-world examples, we don't have precisely known probabilities (what are the chances of finding a match), so we don't know exactly where the "tipping point" is. Still, the principle applies, and that connections enable us to solve problems by the square of the transaction costs to participate in the platform. The paradoxical part is that we underestimate the numerator, the potential solutions that are presented and look solely at the denominator, the low probabilities. Our minds are naturally loss-averse, and we tend to maximize loss potential.
Beyond Connection: High-Probability Platforms
These new high probability platforms architectures will allow a general structure where:
- people and services to find each other,
- where opportunities connect with solutions, take actions,
- participants can share information and
- collaborate on new solutions and try new approaches,
- connect what works and what doesn't (big data analytics) and
- buildi a common body of knowledge, or praxis, that can be constantly refined (eventually I suspect, we'll have a topo map of human health that defines how multipel health measures are connected)
Collaborative platforms are driven by the same statistics as the birthday paradox for connecting on the ability to solve problems, but they then add the ability to modularize large problems into workable, connectable chunks, thereby further reducing risk, and allow for aggregation of data across a wide array of sources, reducing risk even further. It's a triple threat to improving Triple Aim. By matching people, problems and solutions on a platform that enables them to find each other and get work done effectively, amazing things happen with very little top-down control.
Tim O'Reilly puts it aptly in talking about the iPhone in the context of Obama buying into the idea of platforms:
"Before the iPhone, smart phones worked a lot like government procurement. The manufacturers and the carriers got together in a back room and figured out what they thought people needed. Phones came with 20 or 30 apps. But when Apple figured out how to turn the phone into a platform, there were hundreds of thousands of apps delivering ideas that no one at Apple had imagined."
Healthcare today is still in the days of "pre-smartphone" EHRs. When I hear "The manufacturers and the carriers got together in a back room and figured out what they thought people needed. Phones came with 20 or 30 apps." I think of an EHR.
With all the numerous leaks of time and resources in health care, we need an architecture that can support thousands of apps that we can pick or choose, connected over a high-probability architecture. When we provide a platform to provide them at a time and place that's convenient (in mobile that's anytime and almost anyplace), apps find their niche. Because these niches are uncovered through more, better information, increased specialization occurs as developers are fixing smaller and smaller leaks.
Michael Nielsen, in Reinventing Discovery, calls this concept "planned serendipity". Deloitte's John Hagel calls it the "Power of Pull". When this happens, we all benefit from the 80% probability instead of the 10%, all with very little cost of entering the market. Luck is something we make.
So what does this mean for health care IT?
Lower costs on the order of billions of dollars, better care and a better patient experience (what patient doesn't want to connect with the right solution?). It's the Triple Aim of Care, Health and Cost. With the right incentives in place, new architectures can patch the massive number of leaks of time, administration and resources.
One example, ZocDoc, works by putting patients and appointments into a network so that they can find each other. A simple model of leak-fixing with platforms now valued at $700 million.
Then there's everyheartbeat.org, which seeks to track and monitor every heartbeat in the world. What could we find out about our connections when we have this kind of connection? We don't know, but I do know that the birthday paradox will have a role in connecting people's hearts (which may in fact, be inefficient, if not leaking) to find the right heart specialists, and will add up to 1000's of lives saved and millions of dollars working off of the simple math of the birthday paradox.
Simple model: share, connect, collaborate, make better decisions. It's bankable.
What are some of the ways networked health and social media can improve health and make accountable care models successful? Here's just a few, but the possiblities are impossible to predict:
- Finding the right knowledge in the right specialist or expert.
- Collaborating specialists on complex cases.
- Motivation through feedback and social circles for measuring and improving health.
- Finding right disease, right info, right decision and right intervention at the right time. Collective wisdom can match any one wisdom.
- Flexible EHRs and patient-centered platforms allow following the patient and being alerted to interventions beyond the clinic, while allowing for interoperability within it.
- Population health studies that can connect efforts like every heartbeat.org to all sorts of other factors. We could have a real-time picture of how our population health is changing, minute-by-minute.
What don't people get about platforms and social media: connections, information and refinement, combined the right way, mean that problems almost have to find solutions. That often comes across as touchy-feely when people talk excitedly about the opportunities with open source, open data, and social media, but it's really just math. The more you share, the more likely you are to find a match.
Read more on Leonard's blog:
- Ideas Are Cheap ...Until they're shared





Comments are closed.